Abstract
Background
Langerhans cell histiocytosis (LCH) is an orphan disease of clonal dendritic cells, which can affect any organ of the body. There is paucity of data on treatment patterns and outcomes of adult LCH pts, who are usually treated with pediatric-based therapies. No prospective clinical trial has been conducted to date to identify optimal therapeutic strategies in adult LCH. Uncertainty of the natural history of LCH in adults including its pathogenesis, treatment patterns, and outcomes have limited development of novel treatments. Here, we used the Surveillance Epidemiology and End Results (SEER) to describe the epidemiology of LCH, trends in treatment practices over time, and survival outcomes over a forty-year period.
Methods
All 18 registries of SEER covering a period from 1973 to 2014 was used to assemble LCH cohort. LCH cases included in the study had a diagnosis of malignant histiocytosis or LCH (unifocal, multifocal, disseminated, or not otherwise specified). Descriptive data on incidence, demographics, and treatment were collected. Relative survival (RS) was stratified by 5-year (yr) time increments, four age groups [< 20 years (yrs) - pediatric; 20-39 yrs; 40-59 yrs, and > 60 yrs - elderly], and treatment type was estimated using the Kaplan-Meier method and compared between groups using the log-rank test. As LCH pts tend to live longer, we calculated RS probabilities, which compares survival in the pt cohort with the expected survival of the general population having the same characteristics with respect to age, sex, race, and calendar period. Survival probabilities were calculated using the SEER Survival System (SEER*Stat). RS estimates (proportion of cancer pts surviving for a specified period) were calculated by the life table method. Analysis was performed using SEER*Stat.
Results
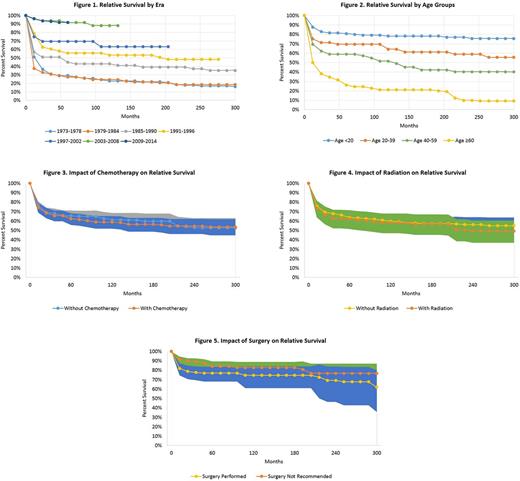
A total of 1480 LCH pts were identified who met the inclusion criteria. Of these, 55% were male, 82% Caucasians, and 58% of cases were diagnosed in the pediatric age group (age <18). The incidence rate remained stable from 1973 to 2009 with an average of 17 new cases per year at an age-adjusted incidence rate of 0.3 per 1,000,000. However, introduction in 2010 of a new International Classification of Diseases code resulted in a significant increase in recorded cases from that year going forth. A variety of treatment modalities were used including 47.8% receiving chemotherapy, 26.2% receiving surgery, and 10.3% receiving radiation therapy. Survival analysis of available SEER data on 705 LCH pts showed a median RS of 16.2 years with 52% of pts alive at 25 yrs. Survival rates have steadily improved since 1973 when assessed in 5-yr increments and since 2003, survival rates have remained steady at 90% (Figure 1). When analyzed by age groups, survival rates successively worsened with advancing age groups with 80% of pediatric pts alive two decades from diagnosis compared to no survivors in the elderly group (Figure 2). In treated pts, receipt of chemotherapy or radiation therapy at diagnosis conferred no survival benefit over those not receiving such treatments (Figures 3 and 4). Likewise, pts receiving surgery at diagnosis did not have significant survival benefit over those not treated with surgery (Figure 5). Notably, 34.1% of the 1480 pts died due to a hematologic malignancy, while 13.1% died due to a solid tumor malignancy. In those who later developed second cancers, there was a significant risk of solid tumor (Odds ratio (OR) 1.69, 95% CI 1.08-2.51, P < 0.05) and hematologic malignancies (OR 4.89, 95% CI 1.96-10.07, P < 0.05).
Conclusion
To our knowledge, this is the first population based study to examine treatment and survival trends in histiocytic disorders, which remain rare and poorly characterized. Notable observations from this study show no relative survival benefit with chemotherapy, radiation therapy, or surgery indicating these treatments were mainly to control local or systemic disease. As such, novel therapeutic approaches are needed to improve outcomes. Although this study shows consistent survival gains since 1973, this is likely due to improvements in supportive care practices. Unfortunately, outcomes in the elderly are dismal compared to pediatric pts. While pts with histiocytic disorders generally have a long duration of remission, we demonstrate that they are at risk for second cancers, particularly hematologic malignancies.
Gerds: Incyte: Consultancy; CTI BioPharma: Consultancy. Advani: Takeda/ Millenium: Research Funding; Pfizer: Consultancy. Sekeres: Celgene: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal